A follow up report on discrimination in B.C.’s health care system is stressing the need to improve access to primary treatment, as too many Indigenous people are forced to seek help in the emergency department due to little access to a family doctor.
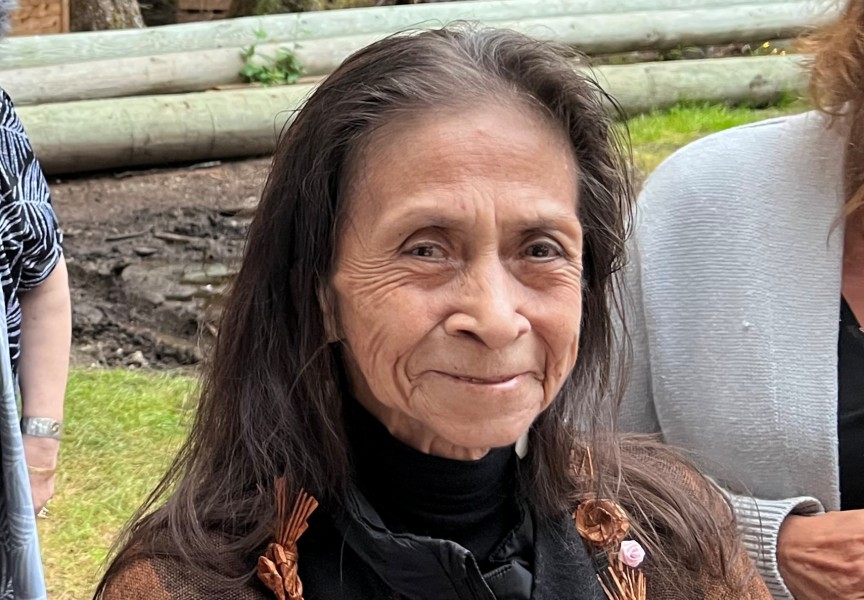
Mary Ellen Turpel-Lafond delivered the report today, after being commissioned by the province to investigate allegations of racism against Indigenous peoples in health care. Her 240-page follow up report is filled with data collected from nearly 9,000 people who helped to inform In Plain Sight: Addressing Indigenous -Specific Racism and Discrimination in B.C. Health Care, which was released on Nov. 30.
The Feb. 4 follow up includes numbers on the high volume of Indigenous patients who rely on emergency services for conditions that often should be treated earlier during routine check ups, said Turpel-Lafond.
“First Nations, on average, are 75 per cent more likely to visit the emergency than anyone else - and the reason for that is that they are not attached to primary care,” said the former judge and provincial child advocate during a Feb. 4 press conference. “Their needs get more acute because they don’t get primary care. And when they go into emergency, it may not be the place to do the referral, to do the communication, to provide the culturally-safe care, because at times emergency departments themselves are in a state of crisis.”
Preventative treatment is being missed, noted Turpel-Lafond, citing pap testing for cervical cancer as an example. Although Indigenous women have a cervical cancer rate that is 1.6 times higher than the rest of the B.C. population, testing for this disease is significantly lower among aboriginal females.
“The health care system in B.C. is a much different experience if you’re an Indigenous person than if you’re a non-Indigenous person,” said Turpel-Lafond. “Instead of having routine health care, we don’t have the continuum; we have the emergency department.”
The lack of access to a general or nurse practitioner is particularly concerning for Indigenous people over 65, according to the follow up report.
“These elders are not attached to primary care at a rate 89 per cent higher than non-First Nations people in British Columbia – and that, in fact, is quite a staggering finding of this data report,” commented Turpel-Lafond. “Poor access to primary care may be driving the lower screening rates for treatable cancers.”
The investigation that informs In Plain Sight began in June, after allegations surfaced that a discriminatory game was being played in at least one B.C. emergency department at the expense of Indigenous patients. Reports claimed that a “Price is Right” competition was being played by emergency room staff, guessing the blood-alcohol content of aboriginal patients as they entered the hospital.
Although Turpel-Lafond did not find evidence of this particular game, in her initial report she found that racism is an “undeniable” problem in B.C. health care, stressing the need for “fundamental changes to beliefs, behaviours and systems” that guide the current services. In Plain Sight has 24 recommendations, including the establishment of an office of the Indigenous health representative and advocate, as well as improvements in the complaint processes facilities use.
During the Feb. 4 press conference Health Minister Adrian Dix spoke of the current overreliance on the ER, a dynamic that has no doubt challenged the province as health authorities struggle to contain COVID-19.
“The fact that so many people around our province - Indigenous people - encounter the health care system through the emergency room and not through primary care is a challenge to our health care system,” he said.